Description
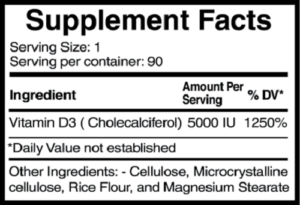
Vitamin D – Dietary Supplement for Postmenopausal Osteoporosis
Maintaining healthy bone density with increasing age is a significant health challenge. Centers for Disease Control and Prevention (CDC) estimates suggest that 9% of U.S. adults over the age of 50 have osteoporosis (per World Health Organization criteria), while nearly half of all adults 50 and older have decreased bone mass. Osteoporosis affects both men and women alike; however, the prevalence is substantially higher in women. The same CDC report estimates that 16% of women have osteoporosis, while 4% of men qualify for this diagnosis. In addition, up to 61% of women aged 50 and older in the United States have decreased bone mass.
Hormonal changes occurring with age as a result of menopause contribute significantly to low bone mass in women. Specifically, decreased levels of estrogen after menopause cause declines in levels of osteoprotegerin (a protein secreted by osteoblasts, the cells responsible for bone building). Osteoprotegerin antagonizes the process of bone resorption (breakdown) that is mediated by osteoclasts (cells responsible for bone breakdown).
Normally, estrogen, when present at premenopausal levels, stimulates the production of bone-building osteoprotegerin, enhancing bone structural density. With menopausal changes and associated reductions in estrogen, however, osteoclast activity is increased, leading to decreased bone mass and, in many cases, postmenopausal osteoporosis in women. Ultimately, this leads to lowered bone mineral density and changes in bone structure, resulting in reduced bone strength and increased risk of fractures.
Lifestyle Strategies for Optimal Bone Density
Menopause-related changes in estrogen levels begin occurring 2–3 years prior to the last menstrual cycle in women, initiating bone loss. The accelerated rate of bone loss continues through menopause for up to 5–10 years. Evidence also suggests that even the lower levels of estrogen in postmenopausal women confer some protection against further acceleration of bone loss by preserving levels of osteoblast activity. Given the prolonged period of bone loss occurring around menopause, however, it becomes more prudent to take measures earlier in life to compensate for this inevitable decrease in bone mineral density.
Peak bone mass is achieved during the third decade of life. While genetic factors have a large influence, modifiable lifestyle and nutritional factors play significant roles in this process.
Of course, no discussion on preventive strategies for osteoporosis can be complete without highlighting the importance of calcium and vitamin D intake, both of which are often low in postmenopausal women. Vitamin D regulates calcium balance. Low intake levels of calcium and vitamin D can induce increased levels of parathyroid hormone, leading to increased bone resorption and an increased risk of fractures. Research suggests that up to 50% of women with osteoporosis may have vitamin D insufficiency.
Try our Vitamin D3 – 5000 IU nutritional dietary supplement in a vegetable capsule.

LEAVE A COMMENT